Health and social care: safe and effective staffing consultation
Consultation on proposals to enshrine safe staffing in law, starting with the nursing and midwifery workload and workforce planning tools.
3 Existing Approaches
Quality health care and workforce planning
3.1 Under the National Health Service (Scotland) Act 1978 NHS Boards in Scotland have a duty to put and keep in place arrangements for the purpose of monitoring and improving the quality of health care which it provides to individuals, and to workforce plan.
3.2 The National Workforce Planning Framework 2005 [17] and the National Workforce Planning Framework 2005 Guidance [18] established the requirement for NHSScotland to workforce plan.
3.3 Revised guidance issued in 2011 [19] sets out the six step methodology to Integrated Workforce Planning and is applied across the whole NHSScotland workforce. In essence, the six steps are:
Step 1 - Defining the plan.
Step 2 - Service Change - what you want to do?
Step 3 - Defining the Required Workforce - what you need to achieve this?
Step 4 - Workforce Capability - what do you have at present?
Step 5 - Action Plan - what needs to happen to deliver the change required?
Step 6 - Implementation and Monitoring.
3.4 Although Integration Joint Boards ( IJBs) are not employers themselves they are required to produce workforce development/organisational development plans. These plans must include (at a minimum) information about the organisational development of NHS Boards, local authorities and IJBs in relation to integration functions, and the arrangements in place to develop and support staff in the delivery of those functions. Nurses and midwives working within IJBs may be employed by the NHS Board, Local Authority or other care provider; therefore, the duty will flow from the employing NHS Board to be discharged by the IJB.
3.5 The Integration Planning Principles which underpin the Public Bodies (Joint Working) (Scotland) Act 2014 also states that the main purpose of services which are provided in pursuance of integration functions is to improve the wellbeing of service-users. It also states that strategic commissioning plans which are developed to deliver integration functions must also protect and improve the safety of service users, within this context the views of Integration Authorities must be taken into account.
Staff governance
3.6 NHSScotland is committed to staff governance and ensuring that all staff feel engaged and valued, contributing to a strong workforce. By investing in a strong workforce, NHSScotland is able to deliver better patient care and continuous improvement in delivering health and care services.
3.7 NHSScotland has a set aim of being an exemplary employer. To help it achieve this, the Staff Governance Standard sets out what staff can expect from their Board and the corresponding responsibilities for all staff. The Staff Governance Standard requires all NHSScotland Boards to demonstrate that staff are:
- Well informed.
- Appropriately trained and developed.
- Involved in decisions.
- Treated fairly and consistently, with dignity and respect, in an environment where diversity is valued.
- Provided with a continuously improving and safe working environment, promoting the health and wellbeing of staff, patients and the wider community.
More information about Staff Governance can be found at: http://www.staffgovernance.scot.nhs.uk/
Staff experience
3.8 NHSScotland is also committed to enhancing the Employee Experience. Improved staff experience should, ultimately, benefit patient care - mechanisms such as staff surveys and the roll-out of iMatter. Staff Experience Continuous Improvement Model is used to find out how staff feel, identify actions required to support staff, address issues to enhance staff experience and, in turn, improve patient care. More information about Employee Experience can be found at:
http://www.staffgovernance.scot.nhs.uk/improving-employee-experience/
Creating an open and honest reporting culture
3.9 We are committed to ensure NHSScotland is a listening organisation. There are a range of mechanisms in place to raise concerns, including discussion with line managers, clinical risk management and incident reporting systems, as well as the Duty of Candour.
3.10 The Duty of Candour procedure, and regulations to be made using the powers combined in the Health (Tobacco, Nicotine etc. and Care) (Scotland) Act, will require organisations to make sure that they are open and honest with people when an unintended or unexpected incident resulting in death or harm has happened. It will also require training and support to be provided for staff involved with disclosure, and support to be available to people who have been affected by an instance of harm. Organisations will be required to prepare an annual report on the duty of candour - this will include a requirement to outline procedures and support available to staff and persons affected by incidents.
3.11 NHSScotland staff should have the confidence to speak up without fear and in the knowledge that any genuine concern will be treated seriously and investigated properly. The Scottish Government in partnership with key stakeholders, has developed a package of measures to promote, encourage and support whistleblowing and whistleblowers in NHSScotland.
3.12 NHS Boards are responsible for ensuring local policies and practice support an open and transparent culture where staff feel it is safe to speak up and concerns can be raised and addressed. These are set out in the Implementing and Reviewing Whistleblowing Arrangements in NHSScotland PIN Policy [20] .
3.13 The NHSScotland Confidential Alert Line ( NCAL) provides an additional level of support to NHSScotland staff should they feel unsure about how or whether to whistleblow.
Existing approaches to nursing and midwifery workforce planning
3.14 The use of evidence based methods and tools is a critical part of making staffing decisions, and ensuring decisions are based on patient care needs, which support effective resource allocation.
3.15 There has been significant financial investment in the NMWWPP since publication of the report in 2004.
3.16 The NMWWPP has made significant progress and we now have a validated framework, methodology and suite of 12 innovative ground breaking workload measurement and workforce planning tools for 98% of NHSScotland nursing and midwifery service areas as detailed below:
- Adult inpatient.
- Mental Health and Learning Disability.
- Neonatal.
- SCAMPS (Paediatric).
- Community Nursing.
- Community Children's and Specialist Nursing.
- Clinical Nurse Specialists.
- Small Wards.
- Perioperative.
- Maternity.
- Professional Judgement.
- Emergency Department/Emergency Medicine - A multi-disciplinary approach has been utilised in the development the Emergency Department/Emergency Medicine ( EDEM) tool which takes account of the workload attributed to both nursing and medical staff rather than being specific only to nursing.
3.17 The tools have been developed utilising robust methodology consistent with the recommendations in the 2004 report and tested extensively across NHSScotland before being confirmed as fit for purpose. Systems and processes are in place to allow collation of data nationally, and an education and a training pack has been developed for professional leaders [21] .
Further information is available at http://www.isdscotland.org/Health-Topics/Workforce/Nursing-and-Midwifery/NMWWP/
3.18 The tools enable evidence based decision making on workforce planning and establishments. The tools do not simply count numbers of patients, but contain formulae - based on rigorous statistical analysis - to calculate the workload attributed to the individual patient. This in turn calculates the Whole Time Equivalent ( WTE) staffing requirement for that workload. For example, the Adult Inpatient tool measures all aspects of work and includes direct and indirect care which is all patient related work, including record keeping, liaison, communications, associated work which includes general non-clinical workload such as clerical, administration, cleaning, stocking, errands, meetings and personal time.
3.19 Quality was also identified as being a key part of nursing and midwifery workload and workforce planning. It is therefore accepted in principle that NHSScotland, in line with best evidence, utilise these approaches as a national standard for workload and workforce planning practice. This principle is often referred to as triangulation. The NHSScotland triangulated approach means that there are three main sets of indicators on which to base judgements (Figure 1). These are obtained from three sources:
- Outcome of the specialty specific workload measurement tool.
- Outcome of the Professional Judgement Tool.
- Quality Measures (in the future these will be identified as part of the Excellence in Care programme of work with specific indicators identified for each of the tools).
Figure 1: Triangulated approach to workload measurement
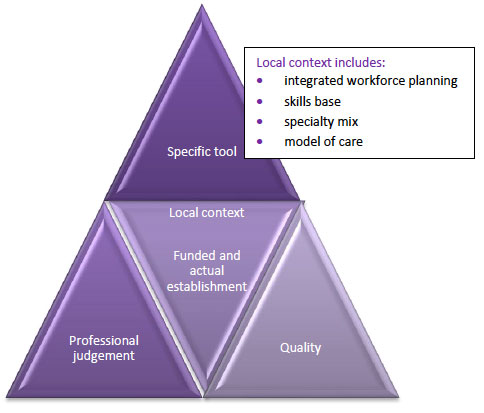
3.20 Other helpful indicators included in the assessment are budget establishment and actual establishment which includes the total nursing and midwifery resource used including supplementary staffing, i.e. bank and agency.
3.21 The process ensures confidence through reliability and validity, and the tools provide Senior Charge Nurses and Midwives, Team Leaders and other managers with a consistent approach upon which to base decisions to support workload, workforce and skill-mix changes. They can also help to identify potential educational needs.
3.22 The workload tools are all available on an IT platform hosted by Scottish Standard Time System ( SSTS). This is accessible to all NHS sites in Scotland and available for use by all registered users. Each ward area, unit and department has been classified as a roster location and it is therefore essential that the information held by SSTS about these locations is accurate. This information includes specialty beds.
3.23 Application of the tools and frequency of use is dependent on the clinical area and patient type. Initially there is an annual review, but this may increase to an 18-24 month review as the tools are embedded in workforce planning arrangements. Service delivery and practice changes may also result in an earlier review if it is felt that the workload tools need further development to keep abreast of change.
3.24 Management Executive Letter ( MEL) 2005 Revised Guidance was re-issued in December 2012 for the development of NHS Board Local Delivery Plans [22] . The guidance mandated the application of available nursing and midwifery workload workforce planning tools as part of Local Delivery Planning. Its aim is to assure Safe, Effective Person-Centred Care across NHSScotland, ensuring that nursing and midwifery workload and workforce planning is consistent, systematic and evidence based throughout the country. Specifically, it stated:
- From April 2014, all Boards will use all available and appropriate workload tools to inform nursing and midwifery workforce planning, this will be evidenced in all Local Delivery Plans from 2014.
- All areas will have used a triangulation process incorporating the use of the Professional Judgement tools and measures of quality to validate the data.
- Local Delivery Plans from April 2014 will contain a paragraph outlining which tools they have used, which areas/wards the tools have been applied to, and the frequency of use.
- The use of nursing and midwifery workload and workforce planning tools and processes to ensure partnership working and frontline staff engagement should be further described within every Board's Workforce Plan narratives and reflected in the projections.
- Out-with the Local Delivery Plan process, Boards should use the appropriate tool to provide information for the required staffing for any new builds, or when as a result of service redesign, a short term pressure, there is a fundamental change to the role, function or location of a service unit or team. This should also follow a triangulation approach.
Current position and future challenges and opportunities
3.25 Although the use of the workload and workforce planning tools has been mandated for Boards since 2013 and the approach is more widely used, there is evidence from the national SSTS platform that indicates incomplete application in all nursing and midwifery job families across NHS Board areas.
3.26 The mandate did not include the requirement to apply the results, evidence analysis, or risk assess the impact that the application of the tools and triangulation process has had on decisions relating to staffing levels, assurance that there is safe and effective staffing or development of workforce plans.
Enshrining safe staffing in law
3.27 In summary, a range of duties and mechanisms are already in place to ensure quality of care, workforce planning and staff governance. Scotland has led the rest of the UK in the development and implementation of evidence-based approaches to nursing and midwifery workload and workforce planning. Significant progress has been made. However, the proposals in this consultation take a further step by placing this approach on a statutory footing to further ensure - and assure - safe and effective staffing.
Contact
Email: Dawn Sungu
Phone: 0300 244 4000 – Central Enquiry Unit
The Scottish Government
St Andrew's House
Regent Road
Edinburgh
EH1 3DG
There is a problem
Thanks for your feedback